Summary
Frozen shoulder often starts quietly, with night pain and a deep ache before real stiffness sets in. For many Ballarat women working from home in their 40s and 50s, early signs show up as trouble reaching overhead or behind the back. Early assessment and gentle support can help reduce pain and limit how much movement you lose over time.
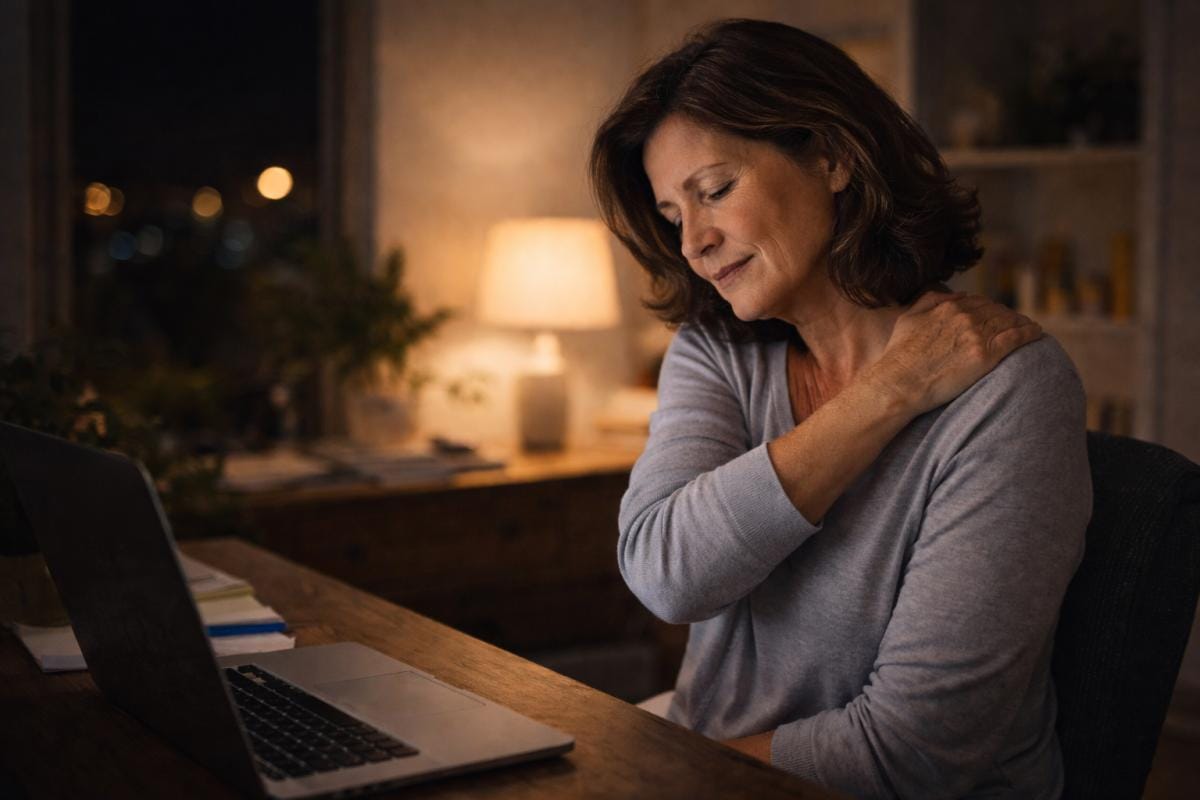
Running a business from home can be brutal on shoulders.
Long hours at a laptop, phone calls squeezed into everything, that habit of scrolling in bed when you finally stop… and then one day you notice it: a deep ache in the shoulder that’s worse at night, and stiffness when you reach up, out, or behind your back.
If you’re a woman in your 40s or 50s, it’s normal to wonder, “Is this frozen shoulder starting?”
Frozen shoulder (adhesive capsulitis) often comes on gradually and is more common in women in midlife. Catching it early matters.
What frozen shoulder actually is (no jargon)
Frozen shoulder happens when the capsule around the shoulder joint becomes irritated and then thickens and tightens over time. The result is a slow combination of pain + increasing stiffness.
It often improves eventually, but the total course can take 1, 3 years for many people (sometimes longer), which is why early support is worth taking seriously.
The 3 stages (and what they feel like in real life)
1) The “freezing” stage (pain builds)
This is where most women first notice something is off.
Common early signs:
- Deep ache in the shoulder that worsens at night and can disturb sleep
- Pain with reaching overhead (putting something on a shelf, hanging washing)
- Pain or stiffness reaching behind your back (bra strap, coat sleeve, tucking in a top)
- A growing feeling that the shoulder is “tight” and not moving freely
This stage can last weeks to months.
2) The “frozen” stage (stiffness dominates)
Pain may settle a bit, but movement becomes much more restricted.
This is often the stage where daily life gets frustrating:
- dressing becomes awkward
- reaching the seatbelt is harder
- driving and turning the wheel can flare it up
3) The “thawing” stage (gradual return of movement)
Pain is usually lower and mobility slowly improves, but it can take many months.
Early warning signs you can check at home (gentle, not aggressive)
These aren’t “diagnostic tests”, but they’re useful clues.
- Behind-the-back reach: can you slide your hand up your spine (like reaching for a bra strap) on both sides? Notice if one side is significantly higher/easier.
- Overhead reach: can you lift the arm up without shrugging hard or twisting your body?
- Side reach: can you reach out to the side without a sharp pinch or deep ache?
If you’re noticing a clear difference side-to-side plus night pain, it’s a good time to get it assessed.
Can WFH posture and phone habits contribute?
They can definitely set the scene for shoulder trouble. Working from home often means:
- shoulders slightly rounded forward
- neck and upper traps staying “on” all day
- fewer natural movement breaks
- more time looking down at devices (which can drive neck/shoulder muscle strain)
That doesn’t mean your phone “causes” frozen shoulder on its own. But it can increase tension, reduce comfortable movement, and make early symptoms louder, especially if you’re already running on stress and poor sleep.
How remedial massage can help in the early phase
Massage can’t “unstick” the shoulder capsule by itself. But in the early stage, it can be very useful support because it can:
- reduce protective tightness in surrounding muscles (neck, upper back, pecs, rotator cuff region)
- ease pain sensitivity around the area
- support circulation and comfort so gentle movement feels more doable
The best results usually come when massage is paired with physio guidance and simple home movement, because shoulder mobility responds well to the right kind of steady input over time.
Important: if your shoulder feels hot, acutely inflamed, or extremely irritable, the work should be gentler, and sometimes you’re better starting with GP/physio input first. (Healthdirect)
A simple “busy woman” action plan (Ballarat-friendly)
If you’re worried you’re in that early freezing stage, aim for small, consistent steps:
1) Warm the shoulder before bed (especially in winter)
Ballarat cold can make everything feel tighter. A warm shower or heat pack for 10 minutes can help the shoulder settle before sleep (comfort first).
2) Make your desk kinder to your shoulders
- bring the screen up closer to eye level
- keep elbows supported (armrests or a cushion)
- drop shoulders away from ears every time you notice them creeping up
3) Micro-movement breaks (2 minutes is enough)
Set a timer for once an hour for micro movements:
- slow shoulder rolls
- gentle chest opening (squeeze shoulder blades softly)
- stand and reach arms forward and up within comfort
4) Get assessed early if it’s affecting sleep or daily tasks
Night pain and growing restriction are the signs that shouldn’t be ignored. (Healthdirect)
When it’s worth seeing your GP promptly
Massage is supportive, but if you have any of these, get medical advice first:
- sudden injury or a fall
- numbness/tingling down the arm
- marked weakness
- severe pain that’s escalating quickly (Healthdirect)
What your first shoulder-focused session can look like
A good remedial appointment for early frozen-shoulder-type symptoms usually includes:
- a quick chat about sleep pain, desk setup, and what movements are hardest
- checking which muscles are guarding (neck, upper back, chest, shoulder)
- targeted work that stays within your comfort level (you shouldn’t feel like you have to brace)
- a simple home plan that fits real life (not a 45-minute routine)
If you’re not sure whether what you’re feeling sounds like early frozen shoulder or “just” shoulder overload from work and life, let your massage therapist know:
- where the pain is
- what time of day it’s worse
- what movements are most restricted
And from there, you will be able to discuss the next best step, massage support, referral to physio, gp, or both.
